Biliopancreatic Diversion (BPD)
Biliopancreatic Diversion (BPD) was developed in the 1970s by Nicola Scopinaro from Genoa, Italy [1].
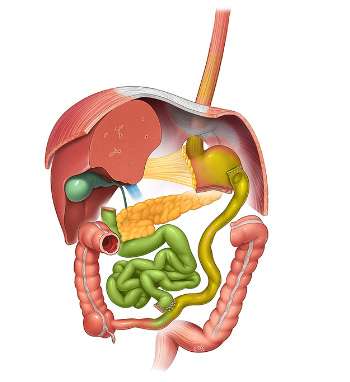
It can be performed laparoscopically and includes three main components:
- Creation of the gastric reservoir. The stomach is transected horizontally to preserve the fundus and proximal part of the stomach body. This reduces the gastric volume to 300 to 500cc and creates a slight restriction of food intake.
- The small bowel is transected at 250cm from the ileo-caecal valve and connected to the proximal stomach. A 2 to 3 cm anastomosis is typically performed to preserve satiety.
- A 50 common channel is created by connecting the biliopancreatic limb to the alimentary limb. A mechanical side-to-side anastomosis is performed and the small bowel opening is closed using running suture.
Procedure
A total of 5-6 trocars are usually required. The operation starts at the level of the proximal gastric body. The lesser sac is entered using blunt peri-gastric dissection. The stomach is then transected horizontally using linear stapler, to bypass its distal two-thirds. In the era of open BPD the distal part (antrum) after a duodenotomy was resected. Background was the prevention of marginal ulcers. Later in the laparoscopic era the antrum and pylorus were preserved without negative side effects.
The common channel is then measured from the ileo-caecal valve and marked using clips or suture at 50. The ileum is then divided at 250 cm from the ileo-caecal valve to create the alimentary limb, and connected to the posterior part of the stomach. The gastro-ileal anastomosis can be performed by different techniques (hand-sewn anastomosis, circular stapler or linear stapler) but should be kept rather small to preserve stomach distension.
A side-to-side ileo-ileal anastomosis is then created at 50 cm from the ileo-caecal valve with a linear stapler. The opening of the anastomosis is closed with absorbable sutures or linear stapling.
In an effort to reduce the complications of Scopinaro's BPD, in 1989 Larrad introduced the modification of lengthening the alimentary channel preserving most of the jejunum-ileum, by creating a short biliopancreatic limb (50 cm) and maintaining 50 cm of common limb (Larrad 50-50 BPD). The longterm results has shown the lowering of hypoproteinemia rate < 0.5% [5],
The mesenteric window and Petersen defect are closed in all variations of the procedure with non-absorbable sutures to avoid internal hernia. Drainage, post-operative nasogastric tube or Foley catheter are not routinely used. Testing of the anastomosis is left to the surgeon’s preference (with methylene blue or with a gastroscope).
Outcomes
BPD is associated with some of the strongest metabolic effects and long-term weight loss of all procedures. Excess weight loss averages 75% at 10 years [2].
Impact on comorbidities, including Type 2 diabetes (resolution rate of 60 to 85%), hypertension (improvement in 60%), sleep apnea (89%) and dyslipidemia (90%) is also well described [3,4]. The effect on hypertriglyceridemia is the strongest of all bariatric procedures. This procedure is however associated with increased gastro-intestinal side-effects, including higher number of bowel movements (average 3 per day), diarrhea, gas bloating and occasional perineal problems (strictures, hemorrhoids and other). Patients need to comply with strict vitamin supplementation, especially fat-soluble vitamins A,D,E and K, and to increase protein intake. Long-term risk of protein malnutrition (4-5%), anastomotic ulcer (2-5%), dumping syndrome and bone demineralization are not uncommon [3,4].
Now a days, sleeve gastrectomy has become the most common bariatric procedure and BPD and its variations are performed less and less during the last decade. With the culture of safety and lowering risks that took place 20 years ago, sleeve gastrectomy has emerged as a procedure of choice. Hence, for super- and super-super-obese patients, there is a tendency these days to perform surgeries in 2 stages, and sleeve is the procedure of choice. Because sleeve is not part of a classic bilio-pancreatic diversion, it is unlikely that this operation will be done as a second stage, making primary BPD unnessary [6].
BPD is still an option after failed VBG (vertical banded gastroplasty) [7]. in The frequency of BPD is worldwide much less than 1%. BPD was never used in USA. BPD has led to the development of the Duodenal Switch variation and to the Single anastomotic duodeno ileostomy (SADI), described in other sections of this website.
References
- Scopinaro N, Gianetta E, Civalleri D et al. Biliopancreatic bypass for obesity: initial experience in man. Br J Surg 1979; 66: 618-20.
- Scopinaro N, Adami GF, Marinari GM et al. Biliopancreatic diversion. World J Surg 1998; 22: 936-46.
- Scopinaro N, Gianetta E, Adami GF et al. Biliopancreatic diversion for obesity at eighteen years. Surgery 1996;119:261-8.
- Bianchi A, Pagan-Pomar A, Jimenez-Segovia M et al. Biliopancreatic Diversion in the Surgical Treatment of Morbid Obesity: Long-Term Results and Metabolic Consequences. Obes Surg 2020;30:4234-4242.
- Larrad-Jiménez A, Díaz-Guerra CS, de Cuadros Borrajo P, Lesmes IB, Esteban BM. Short-, mid- and long-term results of Larrad biliopancreatic diversion. Obes Surg. 2007 Feb;17(2):202-10.
- Gagner M. For whom the bell tolls? It is time to retire the classic BPD (bilio-pancreatic diversion) operation. Surg Obes Relat Dis. 2019 Jun;15(6):1029-1031.
- Daskalakis M, Scheffel O, Theodoridou S, Weiner R. Conversion of failed vertical banded gastroplasty to biliopancreatic diversion, a wise option Obes Surg. 2009 Dec;19(12):1617-23.