Biliopancreatic Diversion with Duodenal Switch
Biliopancreatic Diversion (BPD) was developed in the 1970s by Nicola Scopinaro from Genoa, Italy [1]. The biliopancreatic diversion with duodenal switch (BPD-DS), known as duodenal switch (DS) was created in 1988 by Doug Hess, Bowling Green, Ohio, [2] and was first published by Picard Marceau, Québec, Canada [3] in 1993.
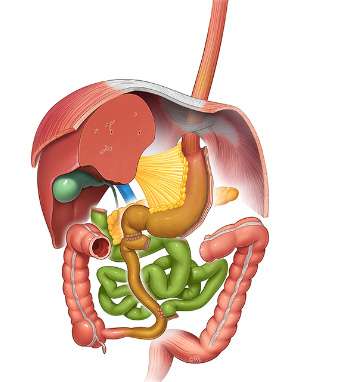
Doug Hess incorporated three main components into the DS:
- Vertical gastrectomy with excision of the greater curvature to significantly reduce gastric volume capacity and provide restriction (a sleeve gastrectomy).
- Division of the duodenum between the pyloric valve and the sphincter of Oddi, preserving the normal function of the pylorus and gastric emptying, to avoid dumping syndrome.
- Bypassing the proximal small bowel results in decreased absorption of nutrients, promoting weight loss. Deriving from experience with BPD the BPD-DS maintains a longer common channel to reduce the risk of vitamin and protein deficiencies.
The first laparoscopic BPD-DS was performed by Michel Gagner in 1999. Laparoscopic Sleeve Gastrectomy (LSG) was initially conceived as the first of a two-step procedure to reduce perioperative morbidity. Subsequently, the sleeve gastrectomy became a stand-alone operation. The size of the Bougie used is however smaller than in BPD-DS, to increase the restriction. Nowadays, SG has become the most popular bariatric operation worldwide.
Procedure
A total of 6 trocars are usually required. The operation starts with a sleeve gastrectomy. For a single-stage BPD-DS, the SG should be large enough to decrease the risk of post-operative malnutrition (ie Bougie size no smaller than 60 French). Hiatal hernias are repaired selectively by most surgeons. Stapling is started 6-7 cm from the pylorus, along the bougie.
The first duodenum is dissected from its posterior attachment and divided with a 60 mm linear stapler 2 to 3 cm distal to the pylorus. Staple-line reinforcement can be useful.
The common channel is measured from the ileo-caecal valve and marked at 75 to 100 cm. The alimentary limb is then divided at 250 cm from the ileo-cecal valve and connected to the post-pyloric duodenum. The duodeno-ileostomy can be performed by different techniques (circular stapled, linear stapled or totally hand-sewn). The hand sewn end-to-side anastomosis is the most common technique and is associated with many benefits (5).
The ileo-ileal anastomosis is created at 75 to 100 cm from the ileo-caecal valve with a linear stapler. The opening of the anastomosis is closed with absorbable sutures. The mesenteric window and Petersen defect are closed with non-absorbable sutures to avoid an internal hernia. Drainage, post-operative nasogastric tube or Foley catheter are not recommended. Testing of the anastomosis is left to the surgeon’s choice (with methylene blue or with a gastroscope).
Outcomes
Duodenal Switch is associated with some of the best long-term weight loss of all procedures, at 40% total weight loss. Resolution of comorbidities, including Type 2 diabetes (90%), hypertension (60%), sleep apnea (70%) and dyslipidemia (90%) is also well described. It is also superior to Roux-en-Y gastric bypass procedure or sleeve gastrectomy for most metabolic complications.
This procedure is however associated with increased gastro-intestinal side-effects, including higher number of bowel movements, bloating, and malodorous gas. Patients need to comply with strict vitamin supplementation and to increase protein intake. Long-term risk of protein malnutrition is not uncommon.
Nowadays, sleeve gastrectomy is the most common bariatric procedure and BPD-DS is more and more performed as a staged operation (SG followed, if needed, 18 to 24 months later by a second-stage DS). A variation of the BPD-DS known as the Single anastomotic duodeno ileostomy (SADI) is described in another section of the website.
References
- S c o p i n a ro N, Gianetta E, C iva l l e ri D et al. Biliopancreatic bypass for obesity: initial experience in man. Br J Surg 1979; 66: 618-20.
- Hess DS, Hess DW. Biliopancreatic diversion with a duodenal switch. Obes Surg 1998; 8: 267-82.
- Marceau P, Biron S, Bourque RA et al. Biliopancreatic diversion with a new type of gastrectomy. Obes Surg 1993; 3: 29-36.
- Chu C, Gagner M, Quinn T, Voellinger DC, Feng JJ, Inabnet WB, Herron D, Pomp A: Two-stage laparoscopic BPD/DS. An Alternative Approach To Super-Super Morbid Obesity. Surgical Endoscopy 2002; S187.
- Weiner, R.A., Pomhoff I, Schramm M, Weiner S, Blanco-Engert R.: Laparoscopic biliopancreatic diversion with duodenal switch: three different duodeno-ileal anastomotic techniques and initial experience. Obes Surg. 2004 Mar;14(3):334-40