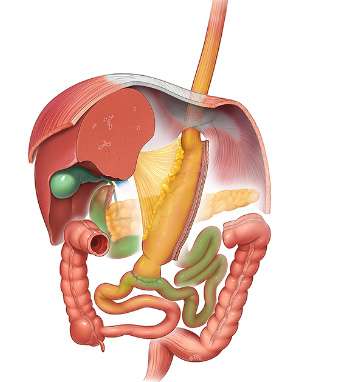
Single Anastomosis Duodenal-Ileal bypass with Sleeve (SADI-S)
Laparoscopic Single Anastomosis Duodenal-Ileal bypass with Sleeve (SADI-S) was first described in 2007 with the intention of simplifying a complex surgical technique, the biliopancreatic diversion with duodenal switch (BPD-DS) (1). Over the years, most studies have demonstrated that SADI-S is a very effective procedure for weight loss and resolution of co-morbidities associated with obesity, like type 2 diabetes, dislypidemia, Obstructive Sleep Apnea (OSA), etc…. (2,3,4). SADI-S has shown good results as primary and as revisional procedure after failed previous operations as well (5,6). Undoubtedly, as all surgical procedures, setbacks have been encountered, although these side effects have been well tolerated and postoperative short and long term complications have appeared to be minimal (2,4,7). These results have driven the ASMBS and IFSO endorsements (8,9).
PROCEDURE (1,4)
A standard laparoscopic approach is performed with four-five ports, with the surgeon positioned between the patient’s legs and the patient remaining in an anti-Trendelenburg position. The optical port is placed 2-3 finger breadths above the umbilicus in the left paramedian line. A left-subcostal port is placed for the surgeon’s right hand, a subxiphoid one is utilized to retract the liver, and a right paramedian port is used for the linear stapler and the surgeon’s left hand. The initial step is to divide all the short gastric vessels and branches of the gastroepiploic arteries to completely dissect the greater curvature of the stomach, from the duodenum to the left crus of the diaphragm.
The duodenum is totally mobilized posteriorly until the gastroduodenal artery and the pancreas are exposed. The duodenal dissection is completed by opening the peritoneum over the hepatoduodenal ligament; the duodenum is then encircled from behind taking care not to damage the right gastric artery.
A large bougie (54 French) intragastric bougie is introduced, and the sleeve gastrectomy is completed with sequential shots of a linear stapler (purple, gold, green or black cartridge) usually protected with some reinforcement material. Then the duodenum is divided with a 60-mm purple/blue linear stapler.
Once both the sleeve and duodenal division are completed, the patient is placed in the horizontal position and the surgeon moves to the left hand side of the patient. The laparoscope is moved to the left subcostal port, and the ileo-cecal junction is identified. 250-300 centimeters are measured proximally along the ileum. At this point, the loop of bowel is lifted up in an ante-colic fashion to the duodenal stump. and an isoperistaltic end-to-side duodenojejunal anastomosis is completed. This can be performed either semi-mechanically with a 30-mm linear stapler or hand sewn with sequential running sutures of a 3/0 absorbable suture. A methylene blue (or air, or endoscope) leak test is then performed. Drain is optional.
OUTCOMES
Weight loss following SADI-S ranges from around 20% EWL in the first 3 months up to nearly 100% after 2 years in some studies, demonstrating a comparable weight loss to that of Roux en Y Gastric Bypass (RYGB) in the mid-term, but showing even superior results in the long-term (2,3,4). These weight loss figures are similar to standard RY-DS.
Metabolic results have been excellent, similar to those reported after any of the previously described biliopancreatic diversions. The reported overall T2D resolution following SADI-S was 60–80% (2,3,4). Dyslipidemia remitted in > 70 % of the cases, OSA in > 80 % and hypertension was controlled in > 60 % with complete remission in > 50 % of the patients (2,3,4).
Protein-caloric malnutrition with procedures such as BPD-DS is an important concern. Nevertheless, SADI-S is an hypoabsorptive technique and these nutritional deficiencies are very uncommon (2,4). When compared with RYGB these abnormalities were similar between both procedures (6), likely related to sufficient postoperative supplementation administered to patients in order to meet their daily requisite of vitamins, minerals and other micronutrients. Regarding quality of life, the mean number of bowel movements after SADI-S ranges about 2.5 per day.
SADI-S is a highly effective as a revisional procedure after failed sleeve gastrectomy (5), and may be an option after other failed bariatric procedures: banding, Vertical Banded Gastroplasty (VBG), or RYGB.
In summary, SADI-s is a hypoabsorptive technique, derived from the biliopancreatic diversion. It is based on the same principles. It is an alternative as an alone surgical procedure for morbidly obese patients and an adequate option as a first step for super-obese patients or high-risk patients.
REFERENCES
- Sanchez-Pernaute A, Rubio Herrera MA, Perez- Aguirre E, Garcia Perez JC, Cabrerizo L, Diez Valladares L. Proximal duodenal-ileal end-to-side bypass with sleeve gastrectomy: proposed technique. Obes Surg. 2007;17(12):1614–8. Doi: 10.1007/s11695-007-9287-8.
- Sanchez-Pernaute A., et al. Single Anastomosis Duodeno–Ileal Bypass with Sleeve Gastrectomy (SADI-S). One to Three-Year Follow-up. Obes Surg. 2010; 20:1720-26. Doi: 10.1007/s11695-010-0247-3.
- Torres A, Rubio MA, Ramos-Leví AM, Sánchez-Pernaute A. Cardiovascular Risk Factors After Single Anastomosis Duodeno-Ileal Bypass with Sleeve Gastrectomy (SADI-S): a New Effective Therapeutic Approach? Curr Atheroscler Rep. 2017 Nov 7;19(12):58. doi: 10.1007/s11883-017-0688-4.
- Surve A, Cottam D, Medlin W, Richards C, Belnap L, Horsley B, Cottam S, Cottam A, Long-Term Outcomes of Primary Single-Anastomosis Duodeno-Ileal Bypass withSleeve Gastrectomy (SADIS), Surgery for Obesity and Related Diseases (2020), doi: https://doi.org/10.1016/ j.soard.2020.07.019.
- Sánchez-Pernaute A, Rubio MÁ, Pérez N, Marcuello C, Torres A, Pérez- Aguirre E, Single-anastomosis duodeno-ileal bypass as a revisional or second-step operation after sleeve gastrectomy, Surgery for Obesity and Related Diseases (2020), doi: https://doi.org/10.1016/ j.soard.2020.05.022.
- Dijkhorst PJ, Boerboom AB, Janssen IMC, et al. Failed sleeve gastrectomy: single anastomosis duodenoileal bypass or Roux-en-Y gastric bypass? A multicenter cohort study. Obes Surg. 2018;28:3834–42. Doi: 10.1007/s11695-018-3429-z.
- Shoar S, Poliakin L, Rubenstein R, Saber AA. Single Anastomosis Duodeno-Ileal Switch (SADIS): A Systematic Review of Efficacy and Safety. Obes Surg. 2018 Jan;28(1):104-113. Doi: 10.1007/s11695-017-2838-8.
- Kara Kallies, M.S., Ann M. Rogers, M.D., F.A.C.S., F.A.S.M.B.S., for the American for Metabolic and Bariatric Surgery Clinical Issues Committee Society. American Society for Metabolic and Bariatric Surgery updated statement on single-anastomosis duodenal switch. Surgery for Obesity and Related Diseases 16 (2020) 825–830
- Brown W, Ooi G, Higa K, Torres A, et al. Single Anastomosis Duodenal-Ileal Bypass with Sleeve Gastrectomy/One Anastomosis Duodenal Switch (SADI-S/OADS) IFSO Position Statement Obes Surg . 2018 May;28(5):1207-1216.