Sleeve Gastrectomy
Find out more about Tube Gastrectomy with the following links.
Laparoscopic Sleeve Gastrectomy (LSG), was first conceived as a first step of a two staged procedure that included a duodenal switch in 2000 (and later Roux-en-Y gastric bypass), and popularized by Dr. M. Gagner. (1) Subsequently, with the use of smaller bougies, the operation was adopted as a primary procedure. Over time the LSG has become the most popular bariatric operation world wide. Most studies have demonstrated that the LSG is effective for weight lossand results in improvement and even resolution of co-morbidities like type 2 diabetes, quite similar to Roux-en-Y gastric bypass, but with less morbidity, and mortality. (2,3)
Procedure
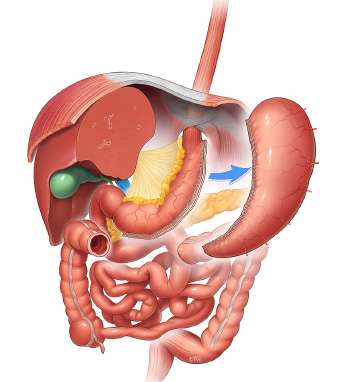
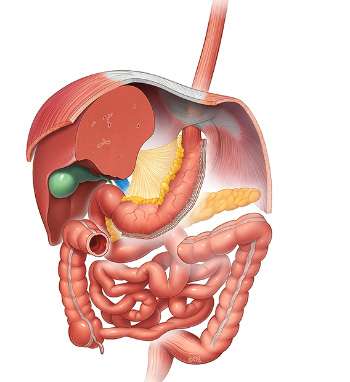
The operation is commenced by using energy devices to take down the greater curvature of the stomach from the antrum to the Angle of His. This includes dividing various branches of the gastroepiploic vessels, close to the gastric wall of the greater curvature. Most operators will fully mobilized the fundus posteriorly, lysing the adhesions in the lesser sac and anterior to the pancreas (more so behind the antrum). The left crus is also exposed to investigate the presence of a hiatal hernia. Most surgeons will selectively close hiatal hernias when identified. Some surgeons will also mobilize the fat pad near the gastro-esophageal junction to better identify this area and staple accordingly. A bougie is introduced trans orally (32-40Fr) and positioned abutting the lesser curvature. The stapling begins 1-6 cm proximal to the pylorus and aiming lateral to the bougie. Strictures are avoided at the incisura angularis by avoiding stapling too close (or tight) to the bougie. One also has to avoid staplingthe esophagus near the GE junction, as most leaks occur distal or near the GE junction. Choosing the appropriate staple height depends on gastric tissue thickness and varies according to the sex, BMI and stomach site. Wall thickness tends to decrease from distal to proximal. Appropriate compression time is necessary, especially in thick tissue. Most surgeons will reinforce the staple line in order to decrease bleeding and leaks. Reinforcement options include suturing orbuttressing. Drainage and leak testing is left to the discretion of the surgeon.
Outcomes
Like the Roux-en-Y gastric bypass, most of the weight loss is achieved in the first 2 years (>70% excess weight loss for BMI less than 50). Weight regain and gastric pouch dilatation can be seen thereafter. At 5 years, there is a sustained weight loss in the range of 50-60% of excess weight.
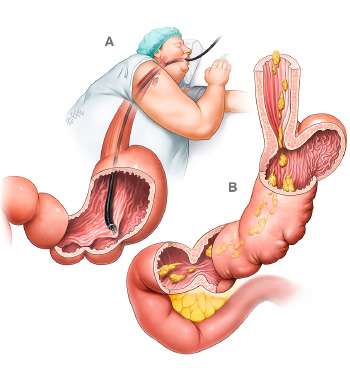
Forsuper-obese patients, a two-stage approach (LSG first followed by completion to a duodenal switch or gastric bypass) has decreased mortality and morbidity from procedures done in one stage. The most feared complication of the LSG is gastric leaks (1-2%), typically occurring several days after surgery and mostly located near the GE junction. Most leaks are now treated with endoscopically placed fully covered nitinol stents, left in place for several weeks, and abscess drainage. GERD reflux is improved in 80% of patients, but in some it may remain or worsen and require prolonged medical therapy or conversion to Roux-en-Y gastric bypass. (4) Weight loss failures can be treated with a variety of surgical optionsincluding re-sleeve gastrectomy, conversion to Roux-en-Y gastric bypass or duodenal switch. (5,6). Appropriate patient selection is important.
References
- Chu C, Gagner M, Quinn T, Voellinger DC, Feng JJ, Inabnet WB, Herron D, Pomp A: Two-stage laparoscopic BPD/DS. An Alternative Approach To Super-Super MorbidObesity. SurgicalEndoscopy 2002; S187.
- Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Brethauer SA, Navaneethan SD, Aminian A, Pothier CE, Kim ES, Nissen SE, Kashyap SR; STAMPEDEInvestigators. Bariatric surgery versus intensive medical therapy for diabetes–3-year outcomes.N Engl J Med. 2014 May 22;370(21):2002-13
- Hutter MM, Schirmer BD, Jones DB, Ko CY, Cohen ME, Merkow RP, Nguyen NT. First report from the American College of Surgeons Bariatric Surgery Center Network: laparoscopic sleevegastrectomy has morbidity and effectiveness positioned between the band and the bypass.Ann Surg. 2011 Sep;254(3):410-20
- Rebecchi F, Allaix ME, Giaccone C, Ugliono E, Scozzari G, Morino M. Gastroesophageal reflux disease and laparoscopic sleeve gastrectomy: a physiopathologic evaluation. Ann Surg. 2014 Nov;260(5):909-14
- Rosenthal RJ; International Sleeve Gastrectomy Expert Panel, Diaz AA, Arvidsson D, Baker RS, Basso N, Bellanger D, Boza C, El Mourad H, France M, Gagner M, Galvao-Neto M, Higa KD, Himpens J, Hutchinson CM, Jacobs M, Jorgensen JO, Jossart G, Lakdawala M, Nguyen NT, Nocca D, Prager G, Pomp A, Ramos AC, Rosenthal RJ, Shah S, Vix M, Wittgrove A, Zundel N.International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of >12,000 cases.SurgObesRelat Dis. 2012 Jan-Feb;8(1):8-19. doi: 10.1016/j.soard.2011.10.019. Epub 2011 Nov 10.
- Gagner M, Deitel M, Erickson AL, Crosby RD. Survey on laparoscopic sleeve gastrectomy (LSG) at the Fourth International Consensus Summit on Sleeve Gastrectomy.Obes Surg. 2013 Dec;23(12):2013-7