Laparoscopic Adjustable Gastric Banding
Introduction
The Laparoscopic Adjustable Gastric Band (LAGB) was introduced into bariatric surgical practice in 1993 as an innovative technique for the treatment of morbid obesity. It involves placing an adjustable band around the upper stomach to induce satiety. The band stoma size can be adjusted by filling the band with sterile saline, which is injected through a port placed under the skin. Long-term adjustments and aftercare are needed to achieve and maintain good outcomes.
How does the LAGB work?
The LAGB reduces appetite. This innovation was not initially realised. The technique was introduced at a time when the simplistic binary concept that all weight loss procedures were restrictive or malabsorptive was current and the LAGB was placed in the restrictive basket. Today we recognize numerous mechanisms may be relevant within each procedure and, for LAGB, control of appetite is first and foremost.
Research study and clinical experience of LAGB have shown that there should be no restriction to the passage of food. For an optimal outcome, each bite of food should have passed across the band within one minute of taking a bite. At the end of a meal there would be no food above the band at one minute after the last bite. The band is not restricting the passage of food.
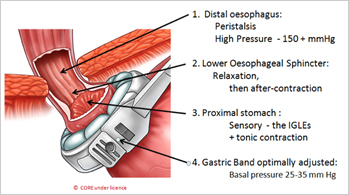
The band is placed at the very top of the stomach. Adjustability is the key to its effect. With optimal adjustment, the band compresses the gastric wall, generating pressure on vagal afferent nerve endings in the myenteric plexus which send signals of satiety to the hypothalamus. During non-eating periods, there is a steady stream of signals passing upwards to maintain a mild sense of satiety throughout the day. During eating, each bite is squeezed across at the level of the band by esophageal and gastric peristalsis to generate multiple stronger signals activating the feeling of satiation. Understanding to detail of this mechanism is essential for optimal adjustment of the band and education of the patient.
1. Placement of the LAGB
The placement of the LAGB is a straightforward outpatient procedure. A detailed description of the technique is provided as Chapter 95 of Fischer’s Mastery of Surgery1. If this book is not available to you, refer to the technique of Ren and Fielding2. There will always be variations between surgeons but some key elements that should be regarded as important are as follows:
- Be gentle. Always do just the minimum dissection to achieve your aims at all stages.
- The two initial dissection points are the peritoneum at the lower aspect of the anterior margin of the right crus and at the Angle of His. The band-placing instrument is passed between these two points.
- The anterior fat pad should be reflected upwards or excised completely unless it is quite trivial. The band must be able to compress directly onto the gastric wall to achieve best effect.
- Place the band across the upper stomach so that the upper border of the band is approximately 1 cm below the esophago-gastric junction. If you are unsure of where the esophago-gastric junction is, use the calibration tube provided with the band. There must be no functional pouch of stomach above the band.
- Achieve secure anterior fixation of the band with 3-4 gastro-gastric sutures.
- Mesh fixation of the port within the subcutaneous fat is an excellent way to get simple and quick placement safely and securely, with minimal post-operative discomfort for the patient and easy and quick access for adjustments in the office. Alternatively, the port can be fixated with sutures to the muscle fascia.
- Patients are usually discharged home with simple analgesics at 2 - 3 hr of completion.
2. 2. LAGB Aftercare
Optimal aftercare is very important component of the LAGB process. The LAGB facilitates correct eating by reducing the appetite through the day and early satiation when eating. Permanent ongoing aftercare is critical to have the band optimally adjusted and to educate and advise the patient regarding best eating practices and other lifestyle changes.
The adjustment of the band is its most attractive feature as it allows gentle but progressive control of appetite. The surgical placement of the LAGB should be seen simply as the first step to the adjustment process. Therefore, to get value from the band, adjustments should be frequent and precise. The decision to adjust is based on the pattern of weight loss and the appetite. For the first year, expect 25% of excess weight loss by 3 months, 38% by 6 months, 45% by 9 months and 50% EWL at 12 months. If your patient is falling below this line, reassess compliance and consider adjustment.
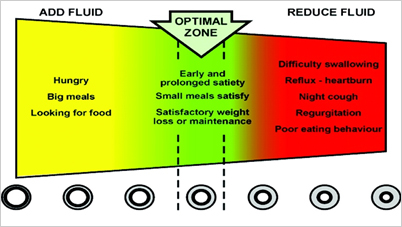
“Green Zone” chart recommended to use to allow patients understand what a correctly adjusted band should feel like (© CORE under licence)
Appetite is assessed by talking with the patient. No imaging is used for decision-making. All adjustments are performed in the office and should take just a few minutes. An initial volume is placed at operation (typically 4 ml for the Lap-Band AP) and increments of 0.1 – 0.5ml are added in the office as indicated.
Eating advice to the patient - The key message to the patient can be summarized in eight words:
“EAT A SMALL AMOUNT OF GOOD FOOD SLOWLY”
There are three key words and three parts to each.
Small Amount:
Three or less meals per day. No snacks. Breakfast is the least important meal of the day.
Half a cup of food (125ml) at each meal.
Use a small fork, small spoon and small plate.
Good food:
Protein-containing
Solid, not liquid, but can be chewed to mush.
Highest quality, tasty, no sugar;
Slowly:
One bite per minute – this is the most important of all the eating rules.
Chew well – maybe 15 – 30 seconds depending on the food
Eat for maximum of 20 minutes – therefore just 20 bites.
Outcomes
With a very long-term follow-up involving over eight thousand patients, O’Brien et al have been able to achieve good weight loss (at 20 years - 49% EWL; 22% total weight loss; 30kg weight loss) safely3. Others have reported similar 20-year outcomes. The 10-year outcomes after LAGB from 17 different groups are provided in reference 3.
- O'Brien P. Laparoscopic Adjustable Gastric Banding. In: J. E. Fischer, ed. Fischer's Mastery of Surgery New York: Wolters Kluwer; 2018(1): 1198-1203.
- Ren CJ and Fielding GA. Laparoscopic adjustable gastric banding: Surgical technique. Journal of Laparoendoscopic & Advanced Surgical Techniques A. 2003;13:257-263.
- O'Brien PE, Hindle A, Brennan L, Skinner S, Burton P, Smith A, Crosthwaite G and Brown W. Long-Term Outcomes After Bariatric Surgery: a Systematic Review and Meta-analysis of Weight Loss at 10 or More Years for All Bariatric Procedures and a Single-Centre Review of 20-Year Outcomes After Adjustable Gastric Banding. Obes Surg. 2019;29:3-14.
